Radiofrequency Ablation (RFA) Treatment in Gynecology
Radiofrequency Ablation (RFA) Treatment in Gynecology: A Safe, Minimally Invasive, Uterus-Preserving Solution for Uterine Fibroids
Introduction
Uterine fibroids (leiomyomas) are one of the most common benign tumors affecting women of reproductive age, often causing heavy menstrual bleeding, pelvic pain, bulk-related symptoms, and infertility. Traditional treatments such as hysterectomy or myomectomy involve major surgery, longer recovery, and potential complications. In response to the growing need for uterus-preserving, minimally invasive, and patient-friendly treatments, Radiofrequency Ablation (RFA) has emerged as a revolutionary option in gynecological care.

What is RFA in Gynecology?
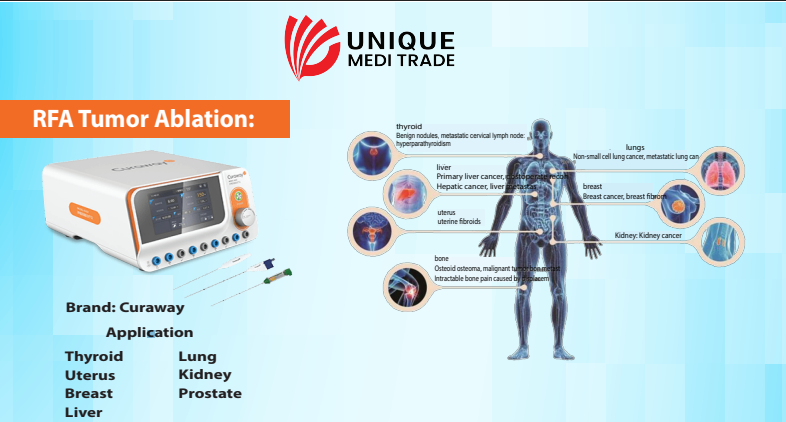
Radiofrequency Ablation (RFA) is a minimally invasive procedure that uses high-frequency energy to generate heat and destroy the fibroid tissue, causing it to shrink over time. The technique is guided by ultrasound or laparoscopic visualization, ensuring precision and safety.
Why Choose RFA for Gynecological Use?
✔ Uterus-Preserving Option
- Allows women to retain their uterus and potential fertility.
- Ideal for women who prefer to avoid hysterectomy or major surgery.
✔ Minimally Invasive and Low-Risk
- Small incision or transvaginal approach.
- Lower risk of complications compared to open surgery or laparoscopic myomectomy.
- Less blood loss and minimal postoperative pain.
✔ Short Recovery Time
- Most patients return to normal activities within 3-5 days.
- Same-day discharge or short hospital stay.
✔ Effective Symptom Relief
- Significant reduction in heavy menstrual bleeding, pain, and pressure symptoms.
- Fibroids shrink gradually over months after treatment.
✔ Clinically Proven & Globally Accepted
- FDA-approved and CE-certified.
- Supported by multiple global clinical guidelines and long-term data.
How is RFA Performed for Fibroids?
- RFA can be performed via laparoscopic, transvaginal, or transcervical approaches depending on the fibroid size, location, and type.
- Under ultrasound guidance, a specialized RF electrode is inserted into the fibroid, delivering controlled thermal energy.
- The fibroid tissue is ablated without affecting surrounding healthy tissue.
- The body naturally reabsorbs the treated fibroid over time.
Indications for RFA in Gynecology
- Symptomatic uterine fibroids (3-10 cm).
- Women seeking uterus-sparing treatment.
- Women who decline or are unfit for major surgery.
- Patients desiring faster recovery and minimal downtime.
Advantages of RFA Over Traditional Treatments
| Aspect | RFA Treatment | Traditional Surgery (Myomectomy/Hysterectomy) |
|---|---|---|
| Invasiveness | Minimally invasive | Major surgery |
| Uterus Preservation | Preserved | Often removed (hysterectomy) |
| Hospital Stay | Same day or 24 hrs | 3-5 days or more |
| Recovery Time | 3-5 days | 4-6 weeks |
| Blood Loss | Minimal | Moderate to high |
| Future Fertility | Potential preserved | Lost (hysterectomy) |
| Complications Risk | Low | Moderate to high |
Clinical Evidence & Safety
-
Multiple studies show 90%+ patient satisfaction rate.
-
Long-term follow-ups reveal significant fibroid shrinkage and symptom control.
-
Minimal recurrence rates when proper patient selection is ensured.
-
Safe for use under global gynecological practice guidelines.
Conclusion
Radiofrequency Ablation (RFA) is transforming the gynecological treatment landscape by offering women a safe, less invasive, uterus-preserving solution for symptomatic uterine fibroids. Its efficacy, patient comfort, short recovery, and global acceptance make RFA a preferred choice among modern gynecologists and patients alike.